Report From a Skilled Nursing Facility
I am a new therapist working on-call at a skilled nursing facility in one of the largest cities in the northeast. Before the COVID-19 pandemic, speech language pathologists, occupational therapists, physical therapists, and the individuals we serve were already navigating a health care crisis based on changes made to how Medicare reimbursed therapy in skilled nursing facilities.
In October, the Center for Medicare and Medicaid Services made it so that facilities would be reimbursed the same amount of money regardless of how many minutes of therapy patients with Medicare received. In theory, this was meant to discourage facility owners from coercing therapists to bill patients for more time than they actually needed. In reality, these new changes financially discourage facilities from providing more than the bare minimum of therapy to patients. The result is a massive loss of jobs for therapists and less skilled therapy for the patients who rely on it in order to return to a safe and independent life.
Most facilities also expect therapists to meet a certain level of productivity. The current standard is that 90% of the time a therapist works should be reimbursable time. That means the amount of time a therapist is writing documentation, going to the bathroom, consulting with other professionals, ordering supplies, cleaning equipment, etc., must account for no more than 10% of their day. That is 48 minutes for an 8-hour workday. These productivity standards exist only so that employers can pay therapists as little as possible while making the most money off them.
How do therapists meet these unrealistic constraints? Here are a few options, you can decide if any of them seem ethical:
1) They see multiple patients at one time. They can accomplish this by providing generic treatments to patients that the patient can perform without the therapist close by. (The more rushed I am, the more time my patients are doing seated dumbbell exercises so I can walk away from them to work with someone else. This is far from the best form of therapy.)
2) They can clock out and then continue to work unpaid. Or work throughout their unpaid lunch break.
3) They may falsify documentation saying they spent more time with a patient or provided different services than they actually did. This is illegal, of course, but I have been encouraged by other therapists or supervisors to bill for time I spend documenting, traveling between rooms, or bill for something that is loosely adjacent to a billable service.
Of course, these sweeping changes happened in October, before the COVID-19 crisis hit the United States. Before the virus we were already struggling to provide quality interventions in an unrealistic amount of time. Now we are also thoroughly sanitizing every piece of equipment between patients. We are only seeing patients in their rooms rather than the therapy gym. This means less opportunity to see multiple patients simultaneously, one of the least unethical ways we prioritize efficiency. While (sometimes quite literally) running between rooms to maintain efficiency, it becomes harder to make sure we are following all the safety protocols necessary to prevent spreading disease between patients.
We are still expected to be 90% productive. This number hasn’t changed. We are forced more than ever to choose between maintaining our rights as workers and making ethical decisions that benefit our patients and keep them safe.
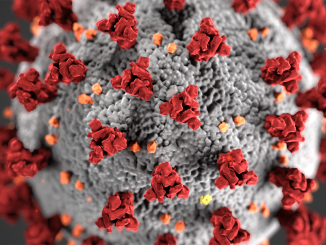
Featured image credit: aldineiderios / Pixabay